

To this end, we developed a mental crisis risk model by inputting EHR data collected over 7 years (2012–2018) from 17,122 patients into a machine learning algorithm.

The underpinning assumption is that there are historical patterns that predict future mental health crises and that such patterns can be identified in real-world EHR data, despite its sparseness, noise, errors and systematic bias 33. This research explores the feasibility of predicting any mental health crisis event, regardless of its cause or the underlying mental disorder, and we investigate whether such predictions can provide added value to clinical practice. Furthermore, even a highly accurate predictive model does not guarantee improved mental health outcomes or long-term cost savings 29, 30 therefore, it remains unclear whether new predictive technologies could provide tools that are useful to mental healthcare practitioners 31, 32. This would enable optimizing healthcare staff allocation and preventing crisis onset. Much remains unknown about the feasibility of querying machine learning models continuously to estimate the risk of an imminent mental health crisis. However, the mental health literature is limited to predicting specific types of events-such as suicide, self-harm and first episode psychosis 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28-rather than continuously predicting the breadth of mental health crises that require urgent care or hospitalization. Research has already demonstrated the feasibility of predicting critical events associated with a wide range of healthcare problems, including hypertension, diabetes, circulatory failure, hospital readmission and in-hospital death 11, 12, 13, 14, 15, 16, 17. Thus, shifting such tasks to the automated analysis of electronic health records (EHRs) holds great promise to revolutionize health services by enabling large-scale continuous data review.
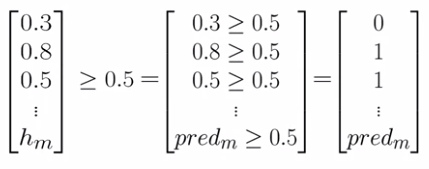
Logistic regression flaticon manual#
In busy clinical settings, the manual review of large quantities of data across many patients to make proactive care decisions is impractical, unsustainable and error-prone 10. Therefore, identifying patients at risk of experiencing a crisis before its occurrence is central to improving patient outcomes and managing caseloads 9. By this point, it is too late to apply preventative strategies, limiting the ability of psychiatric services to properly allocate their limited resources ahead of time. However, patients are frequently already experiencing a mental health crisis when they access urgent care pathways as their primary entry point to a hospital or psychiatric facility. Timely treatment can prevent exacerbating the symptoms that lead to such crises and subsequent hospitalization 8. In clinical practice, considerable demand arises from mental health crises-that is, situations in which patients can neither care for themselves nor function effectively in the community and situations in which patients may hurt themselves or others 6, 7.
With the global mental health emergency considerably exacerbated by the Coronavirus Disease 2019 pandemic, healthcare systems face a growing demand for mental health services coupled with a shortage of skilled personnel 2, 3, 4, 5. Nearly 1 billion people worldwide live with a mental disorder 1. To our knowledge, this study is the first to continuously predict the risk of a wide range of mental health crises and to explore the added value of such predictions in clinical practice. A follow-up 6-month prospective study evaluated our algorithm’s use in clinical practice and observed predictions to be clinically valuable in terms of either managing caseloads or mitigating the risk of crisis in 64% of cases. The model achieves an area under the receiver operating characteristic curve of 0.797 and an area under the precision-recall curve of 0.159, predicting crises with a sensitivity of 58% at a specificity of 85%. Therefore, we developed a machine learning model that uses electronic health records to continuously monitor patients for risk of a mental health crisis over a period of 28 days. However, the high prevalence of mental health problems means that the manual review of complex patient records to make proactive care decisions is not feasible in practice. The timely identification of patients who are at risk of a mental health crisis can lead to improved outcomes and to the mitigation of burdens and costs.


 0 kommentar(er)
0 kommentar(er)
